VAGINAL DRYNESS
Vaginal Dryness is a common but with painful symptoms that many people may experience at some point during their lives. It affects both pre-and postmenopausal women at any age.
REASONS FOR VAGINAL DRYNESS
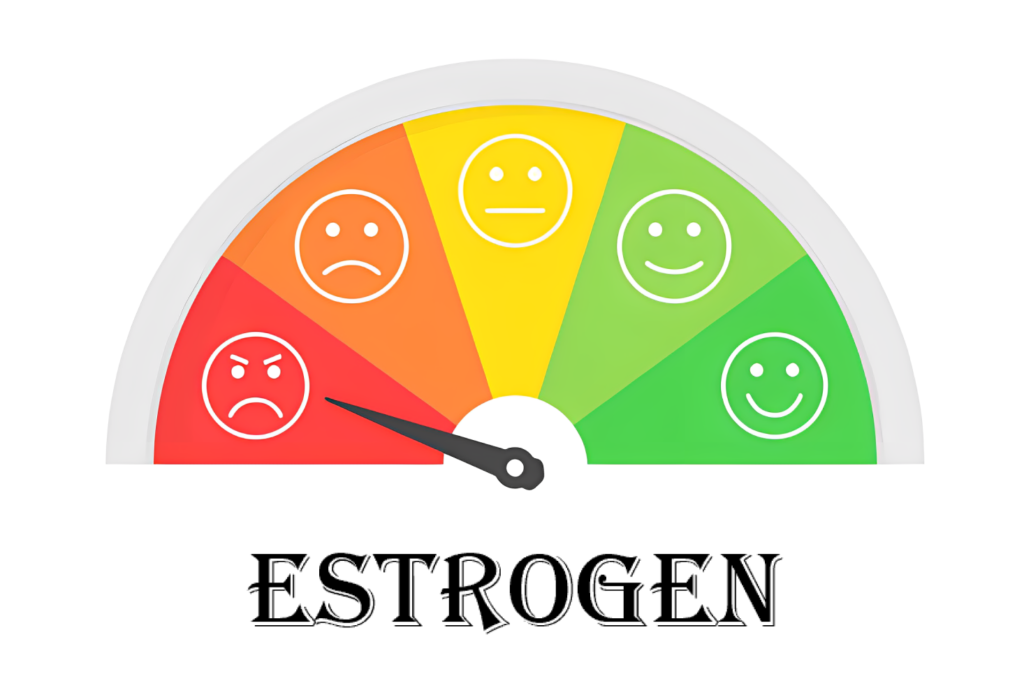
- Under normal conditions, the walls of the vagina are lubricated with a thin layer of clear fluid; the hormone estrogen helps maintain the fluid and keeps the lining of the vagina healthy, thick, and elastic.
- Vaginal dryness occurs when the lining of the vagina becomes thin, dry, and lacks proper moisture.
- A decrease in estrogen levels can lead to a reduction in the amount of moisture available in the vagina.
- The decline in estrogen can occur at any age and may result from various causes, conditions and factors, including menopause, certain medications, and breastfeeding.
- In premenopausal women, vaginal dryness is related to hormonal down-regulation. However, the affected women prefer not to talk about the problem openly due to lack of health literacy.
COMMON SYMPTOMS OF VAGINAL DRYNESS
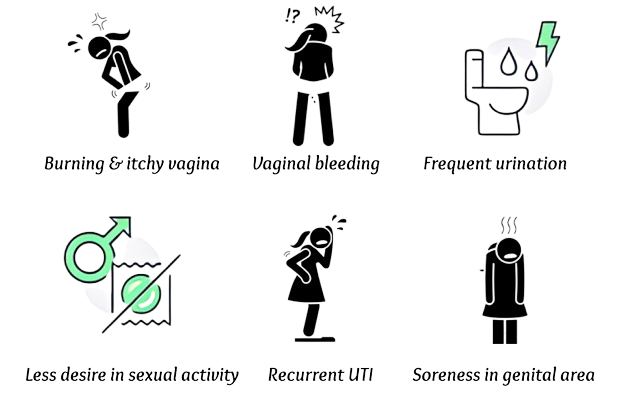
- Burning and itching in the vaginal area.
- Bleeding after sex due to vaginal wall tissues becoming fragile and breaking open.
- Soreness in the vulva, the external genital area.
- Recurrent urinary tract infections (UTIs) including yeast infections.
- Frequent urination.
- Decreased desire or lack of interest to engage in sexual activity.
Less moisture in your vagina leads to less moisture in your vulvar area (external genitals) and it can make you feel the dryness or irritation:
- While clothing or putting on your underwear.
- During normal activities like walking or sitting.
Vaginal Dryness
Manifestation
- Initially, vaginal dryness may present as a minor irritation or discomfort.
- However, it can progress to cause significant pain and discomfort during activities such as sitting, exercising, urinating, and sexual intercourse.
- The sensation of dryness in the vagina can result in burning, itching, and soreness in the genital area.
- The resulting pain and discomfort can have a substantial impact on a person's quality of life, affecting their overall well-being and daily activities.
PREVALENCE OF VAGINAL DRYNESS
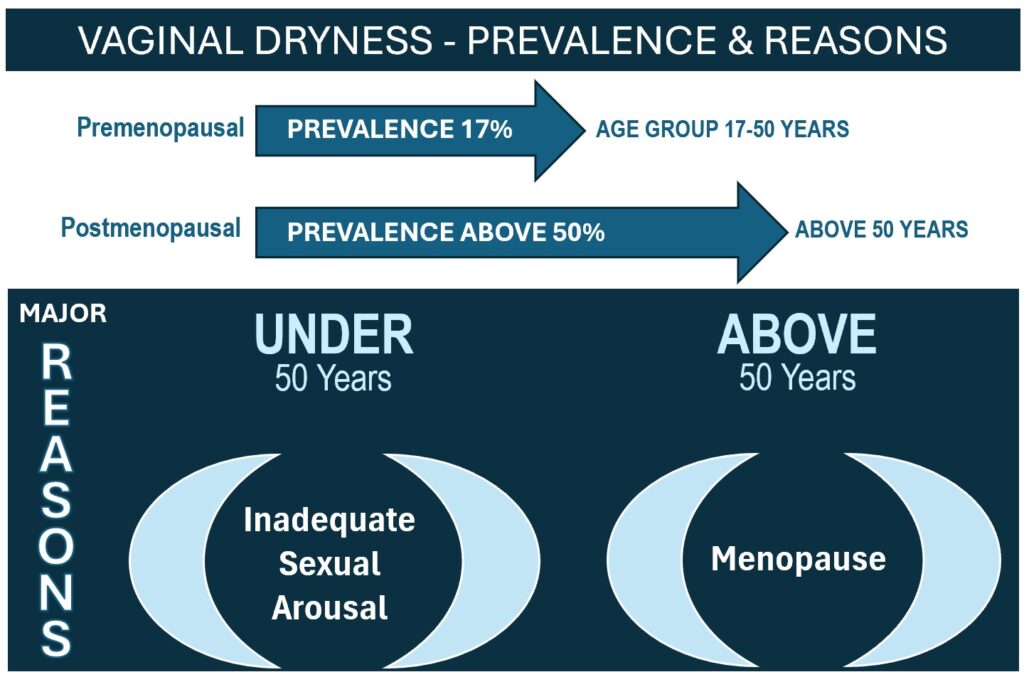
- Vaginal dryness is commonly associated with postmenopausal women due to the decline in estrogen levels that occurs during menopause.
- However, it is important to note that vaginal dryness can occur in premenopausal women.
- Approximately 17% of premenopausal women between the age group of 17 to 50 years experienced problems with sexual intercourse, due to vaginal dryness.
- Prevalence of self-reported vaginal dryness varied from among women, 5.8% in Italy to 19.7% in Brazil.
- The majority of women under 50 attributed vaginal dryness to inadequate sexual arousal while women over 50 believed it was because of aging or menopause.
- In postmenopausal women, more than half of the population suffers from mild to severe vaginal dryness related to the decreasing level of estrogen.
- In an Indian study, vaginal dryness was found to be an important problem with more than 50% of postmenopausal women reporting it.
POSSIBLE CAUSES OF VAGINAL DRYNESS
Vaginal dryness can result from
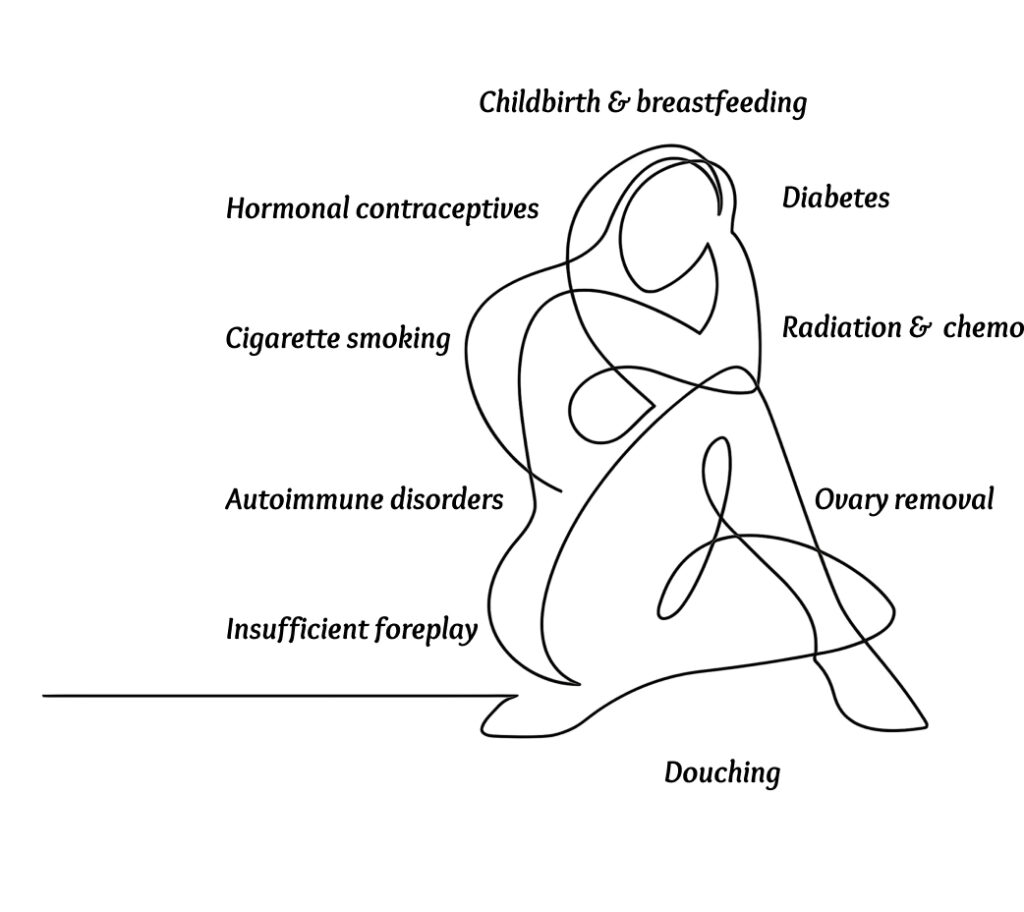
| Childbirth and breastfeeding: | Hormonal changes during pregnancy and breastfeeding can alter the vaginal environment, making it more susceptible to vaginitis. |
| Use of birth control pills or other hormonal contraceptives: | Hormonal contraceptives can disrupt the natural balance of the vaginal microbiota, increasing the risk of vaginitis. |
| Cigarette smoking: | Smoking has been linked to an increased risk of vaginal infections and can impair the immune response, making it more difficult to fight off infections. |
| Use of certain medications: | Some medications, such as antidepressants and antihistamines, can cause increase the risk of vaginitis. |
| Autoimmune disorders: | Autoimmune conditions like Sjogren’s syndrome that attack moisture-producing cells in the body can lead to vaginal dryness and an increased risk of vaginitis. |
| Douching: | Using soaps, sprays, or washes around or inside the vagina can disrupt the natural vaginal flora and pH balance, increasing the vulnerability to vaginitis. |
| Diabetes: | Poorly controlled diabetes can lead to elevated glucose levels in vaginal secretions, creating an environment favorable for the growth of yeast and bacteria. |
| Anti-estrogen medications: | Certain medications used for conditions like uterine fibroids or endometriosis can cause hormonal changes and vaginal dryness, increasing the susceptibility to vaginitis. |
| Radiation, chemotherapy, or hormone therapy for cancer treatment: | These treatments can impact the vaginal tissues and disrupt the normal vaginal environment, leading to an increased risk of vaginitis. |
| Surgical removal of the ovaries: | The removal of ovaries can result in hormonal changes and vaginal dryness, increasing the susceptibility to vaginitis. |
| Insufficient foreplay before sexual intercourse: | Inadequate foreplay can result in insufficient vaginal lubrication, leading to irritation and an increased risk of vaginitis. |
THE OUTCOME OF VAGINAL DRYNESS
- Vaginal dryness, regardless of its cause, can cause significant discomfort and unpleasant symptoms.
- Common issues associated with vaginal dryness include itching, burning, and pain during intercourse (dyspareunia).
- Dryness in the vulva, the external genital area, can lead to irritation and discomfort, especially when in contact with clothing or innerwear.
- Some women may also experience increased urinary frequency or an increased risk of urinary tract infections (UTIs) alongside vaginal dryness.
DIAGNOSIS OF VAGINAL DRYNESS
When evaluating vaginal dryness, healthcare providers examine the medical history including the medications taken, and perform various diagnostic tests and examinations, including:
| Pelvic exam: | The healthcare provider examines the vagina to assess its condition. In cases of vaginal dryness, the vaginal lining may appear thin, dry, and red |
| Blood test for Hormone: | To measure hormone levels, such as estrogen, to determine if hormonal imbalances contribute to vaginal dryness |
| Other Blood tests: | If a specific medical condition is suspected, blood tests may be ordered to identify and assess that condition. |
| Infection screening: | Testing may be performed to check for signs of infection, such as a vaginal swab to analyse the sample of vaginal discharge. |
These tests and examinations are aimed at identifying the underlying cause of vaginal dryness and guiding appropriate treatment options.
TREATING VAGINAL DRYNESS
Many options are available for the treatment of vaginal dryness and painful intercourse (dyspareunia) associated with vaginal dryness.
LUBRICANTS AND MOISTURIZERS FOR VAGINAL DRYNESS
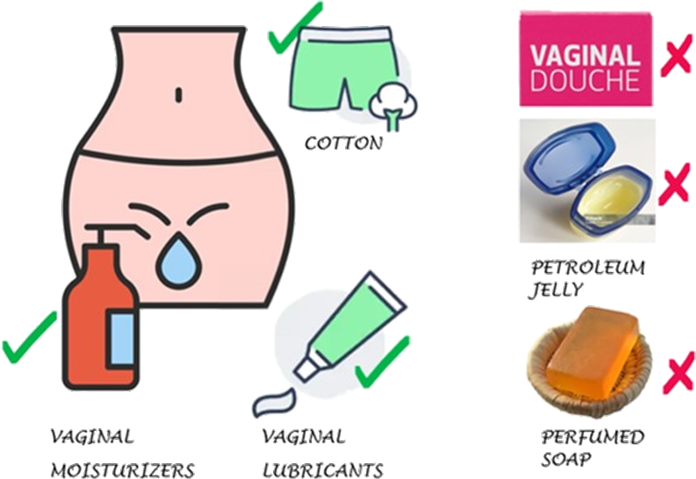
- Vaginal lubricants and moisturizers are commonly used for vaginal dryness. Using it replenishes the vaginal tissues, and makes it wet to address the pain during sex.
- Moisturizers meant for the face or body shouldn’t be used for vagina dryness.
| VAGINAL MOISTURIZERS: Apply vaginal moisturizers to the inside of your vagina to keep your vaginal lining healthy. |
| VAGINAL LUBRICANTS: Apply lubricants just before sexual intercourse to ease discomfort caused by sex |
MEDICATIONS FOR VAGINAL DRYNESS
- Medication for vaginal dryness should be used only on the recommendation of a Medical Practitioner to avoid the associated risk.
- Most of the medication acts like the hormone estrogen and is prescribed based on its safety and efficacy.
ESTROGEN CREAM, RING, OR TABLET
- These medications work by providing estrogen. Creams and tablets are applied directly into your vagina using an applicator.
- Estrogen-containing rings are placed into your vagina to release a steady stream of estrogen directly to the tissues and are usually replaced every 3 months.
CAUTION: Estrogen-containing products have side effects. It may cause vaginal bleeding, breast pain, etc., and should be used only under medical supervision.
Topical application of estrogen may not be recommended in conditions like
- Pregnant
- Breastfeeding
- Breast cancer
- History of endometrial cancer
- Vaginal bleeding
GENERAL PRECAUTIONS RECOMMENDED FOR VAGINAL DRYNESS
- Use of unperfumed soaps and washes around your vagina
- Use of water-based lubricants in and around your vagina before sex
- Longer foreplay to get more arousal during sex
- Not recommended to put creams or lotions like petroleum jelly inside your vagina to avoid infection
- Not to use face and body moisturizers
- Not to use any douches
WHEN TO CALL THE DOCTOR
A dry vagina is usually not a sign of a serious medical condition. But seeking medical attention is recommended in below conditions when vaginal dryness:
- Interferes with your daily activities.
- Affects your sex life.
- Doesn’t get better with over-the-counter treatments.
- Unusual discharge from your vagina
- Severe vaginal bleeding

